When embarking on the journey of fertility treatment, understanding the various gynaecological factors that can influence success is crucial.
This knowledge empowers you to make informed decisions and increases your chances of achieving the desired outcome. Let’s explore the key gynaecological factors that can affect fertility treatment success.
Age and Ovarian Reserve
Your age is a significant factor in fertility treatment. As you age, both the quality and quantity of your eggs decline, impacting your fertility. This decline becomes more pronounced after the age of 35.
To assess your ovarian reserve, tests such as Anti-Müllerian Hormone (AMH), Follicle Stimulating Hormone (FSH), and Antral Follicle Count (AFC) are used. These tests provide insight into your egg supply and help tailor your fertility treatment plan.
Uterine Abnormalities
Uterine abnormalities, whether congenital or acquired, can impede implantation and pregnancy maintenance. Conditions like a septate uterus or bicornuate uterus are congenital, meaning you are born with them.
Acquired abnormalities such as fibroids, polyps, and adhesions can develop over time. Addressing these issues through surgical or medical interventions can improve your chances of a successful pregnancy.
Polycystic Ovary Syndrome (PCOS)
PCOS is a common hormonal disorder that affects ovulation. Symptoms include irregular periods, excess androgen levels, and polycystic ovaries. This condition can lead to anovulation, where you do not ovulate regularly.
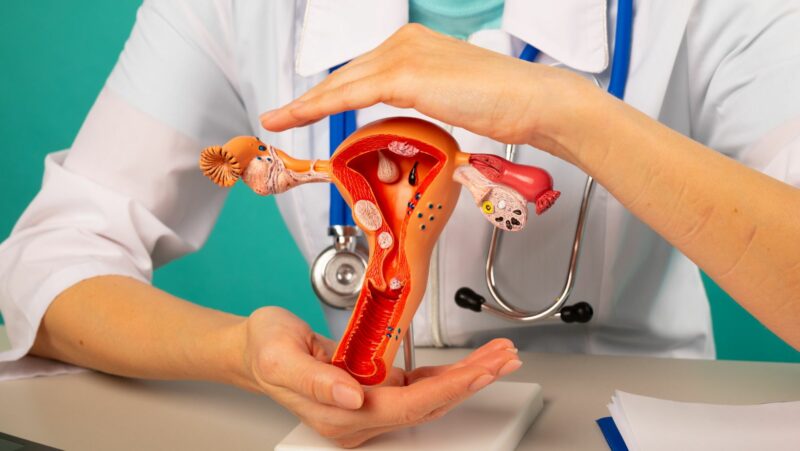
Lifestyle changes, medication, and ART can help manage PCOS and improve your chances of conception. Additionally, your IVF clinic can provide tailored treatment plans to address PCOS-related fertility issues.
Tubal Factors
Your fallopian tubes play a critical role in natural conception. Tubal blockages, often caused by infections or conditions like endometriosis, can prevent the sperm and egg from meeting.
Hydrosalpinx, a condition where fluid accumulates in the fallopian tubes, can negatively affect IVF success. Diagnostic tests like Hysterosalpingography (HSG) or laparoscopy are used to evaluate tubal patency and guide treatment decisions.
Endometriosis
Endometriosis is a condition where tissue similar to the lining of your uterus grows outside it, causing pain and infertility. It affects ovarian function and the pelvic environment, making conception more challenging.
Treatment options include medication, surgery, and assisted reproductive technologies (ART) like IVF. Managing endometriosis effectively can enhance your fertility treatment outcomes.
Pelvic Inflammatory Disease (PID)
PID is an infection of the reproductive organs that can result in long-term damage, including tubal blockages and adhesions. Early treatment and prevention of PID are essential to protect your fertility.
If you have a history of PID, your fertility specialist may recommend specific treatments to address any resulting complications.
Previous Gynaecological Surgeries
Surgeries like myomectomy (removal of fibroids) or ovarian cystectomy (removal of ovarian cysts) can impact your reproductive organs. Understanding the effects of these surgeries on your fertility is important.

Your fertility specialist can guide you on the best approach to maximize your chances of a successful pregnancy post-surgery.
Closing Statement
Understanding these gynaecological factors can greatly improve your chances of fertility treatment success. By addressing these issues proactively, you can take control of your fertility journey and increase your chances of achieving a successful pregnancy.